Abstract
Background/Objective: Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, progressive, potentially life-threatening, hematologic disorder characterized by uncontrolled activation of the terminal complement pathway; it often occurs in patients with underlying bone marrow failure (BMF), most commonly aplastic anemia (AA). The presence of both diseases may present challenges to clinicians regarding optimal patient management. The International PNH Registry is a prospective, observational study of patients with PNH regardless of treatment with eculizumab, a humanized monoclonal antibody that blocks terminal complement activation at C5. The objective of this analysis was to evaluate clinical and laboratory outcomeswith eculizumab in patients with PNH, with or without history of AA. The analysis was restricted to the subpopulation of patients with high disease activity (HDA) to allow for an appropriate assessment of eculizumab-related treatment effects in the presence or absence of a history of AA in the setting of PNH.
Methods: Eculizumab-treated patients with HDA at initiation of therapy in the Registry were stratified by history of AA as reported by their treating physicians. HDA was defined as evidence of hemolysis (elevated lactate dehydrogenase [LDH] ratio ≥1.5 x upper limit of normal) and presence of any PNH-related symptoms, including fatigue, hemoglobinuria, abdominal pain, dyspnea, anemia (hemoglobin <100 g/L), major adverse vascular event (MAVE; including thrombotic event [TE]), dysphagia, or erectile dysfunction. Patients were assessed at baseline (defined as the date of eculizumab initiation) and at last follow-up. Outcomes were assessed in patients with at least 6 months of follow-up time after initiation of eculizumab and included rates of MAVE, TE, and red blood cell (RBC) transfusions received before and after baseline, and changes from baseline to last follow-up in laboratory values.
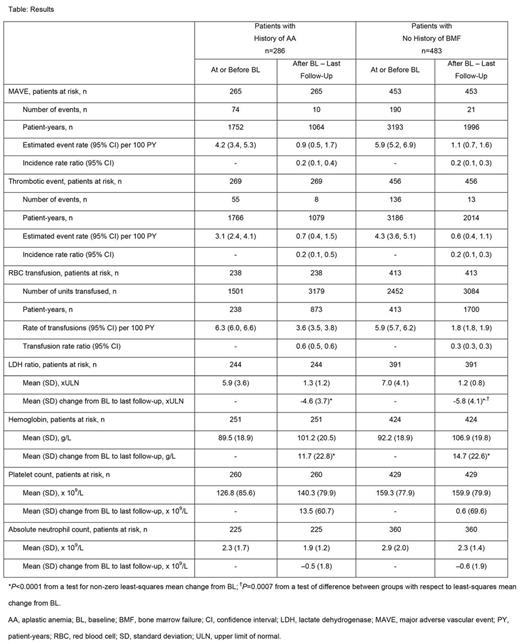
Results: As of June 5, 2017, 4928 patients were enrolled in the Registry. Of these, 769 patients with HDA, treated with eculizumab, with non-missing data on demographics, enrollment date, and BMF status, and with ≥6 months of follow-up were included in these analyses. Of these, 286 (37%) had a history of AA at initiation of eculizumab (including 223 [78%] reported as ongoing AA), and 483 patients (63%) had no history of any BMF. Median (min, max) follow-up on treatment was 3.6 (0.5, 12.0) and 4.0 (0.5, 12.0) years in patients with history of AA and without any history of BMF, respectively. The majority of patients in both the history of AA group and the group without any history of BMF had >50% glycosylphosphatidylinositol-deficient granulocytes at baseline (82% and 93%, respectively); median (Q1, Q3) LDH ratio at baseline was 4.9 (3.0, 7.5) and 6.2 (3.7, 9.0), respectively. Treatment with eculizumab was associated with substantial improvement in the rates of MAVE, TE, and RBC transfusion as well as a significant reduction from baseline in mean LDH ratio, regardless of whether patients had history of AA at initiation of eculizumab (Table).
Conclusions: Eculizumab treatment was associated with significant improvement in clinical and laboratory outcomes related to PNH, regardless of AA history. Findings from this analysis suggest that history of AA does not adversely impact the effectiveness of eculizumab in patients with PNH. Our findings are consistent with the notion that patients with PNH who have HDA, including those with history of AA, should be treated with eculizumab.
Peffault De Latour: Amgen: Research Funding; Novartis: Consultancy, Honoraria, Research Funding; Alexion Pharmaceuticals, Inc.: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy, Honoraria, Research Funding. Brodsky: Alexion Pharmaceuticals, Inc.: Membership on an entity's Board of Directors or advisory committees, Other: Grant Funding. Hill: Alexion Pharmaceuticals, Inc.: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees. Roeth: Alexion Pharmaceuticals, Inc.: Consultancy, Honoraria; Roche: Consultancy, Honoraria. Schrezenmeier: Alexion Pharmaceuticals, Inc.: Honoraria, Other: Research Funding to University of Ulm . Wilson: Alexion Pharmaceuticals, Inc.: Employment, Equity Ownership. Marantz: Alexion Pharmaceuticals, Inc.: Employment, Equity Ownership. Maciejewski: Alexion Pharmaceuticals, Inc.: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Speaker Fees; Ra Pharma: Consultancy; Apellis Pharmaceuticals: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal